Esophageal Atresia
Esophageal atresia is an abnormality, or birth defect, of the esophagus that occurs early in pregnancy, as the baby is developing. The esophagus forms in the first few months of fetal life as a long, hollow, continuous tube joining the mouth to the stomach. In newborns with this birth defect, formation of this continuous esophageal tube is interrupted.
In most cases, two separate tubes are formed, an upper (proximal) tube connected to the mouth and a lower (distal) tube connected to the stomach. This seperated tubes are sealed off creating a pouch on either side; the gap between these pounches can be short or very long. Saliva can accumulate in the upper pouch as it cannot drain into the stomach.
Tracheoesophageal Fistula
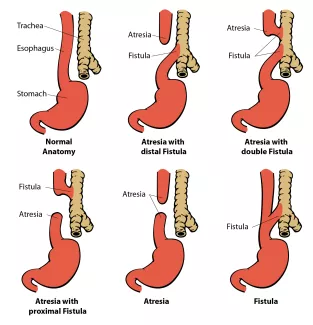
Newborns with esophageal atresia often also have a tracheoesophageal fistula which is a direct connection between the esophagus and the trachea (windpipe). Most commonly with esophageal atresia, this connection forms off of the lower (distal) pouch; however, it can also form off of the upper pouch or both, and in some cases, a fistula will form without atresia. The tracheoesophageal fistua can lead to breathing problems (aspiration pneumonia), if saliva from the upper pouch, or stomach contents from the lower pouch, enter the trachea and lungs.
In newborns with EA/TEF, the trachea may also be affected by a condition known as tracheomalacia. This means the trachea is softer and less rigid than normal. This varies in severity from child to child. This can contribute to a "barking cough." This is expected to improve as the child grows older. Sometimes tracheomalacia is severe and requires additional treatment.
Varients of Esophageal Atresia & Tracheoesophageal Fistula
How is esophageal atresia & tracheoesophageal fistula treated?
Your baby will be cared for in an Intensive Care Nursery by specially trained doctors and nurses. If a tracheoesophageal fistula is present, it must be surgically closed soon after birth. During fistula closure, if the gap between the two ends of the esophagus is small, they will be sewn together and the esophageal atresia will be repaired. This is called a primary repair. If the upper and lower pouches are too far apart to bring together, only the fistula will be closed and the repair of the esophagus may be delayed. If the gap is very wide, an alternative method of surgical repair of esophageal atresia may be offered. This will be discussed with you by your child's Pediatric Surgeon.
Before the esophagus is repaired, saliva can accumulate in the upper pouch, and may spill into the lungs. This can lead to choking. To prevent choking a small tube, attached to suction, is passed through the mouth into the upper pouch to provide continuous drainage of saliva.
At the time of esophageal repair, a tube will be placed in your child's chest to drain any fluid that might accumulate near the surgical site. Several days after surgery a special x-ray, called a contrast esophagram, will be performed. This test is done to ensure there are no leaks along the esophageal repair. If the incision has healed, without a leak, the chest tube will be removed and feedings will be started by mouth. In some cases the esophageal repair may take longer to heal, and a leak will be visible on the x-ray study. If there is a leak, the chest tube will remain in place until the leaking stops. X-ray studies will be repeated every several days until the esophageal repair has completely healed.
How will my baby be given feedings?
 Intravenous fluids will be given until breast milk or formula feedings can be started. Feedings are begun once your baby has recovered from the operation, usually after several days. Feedings will be given one of two ways. If the esophagus is repaired primarily, a thin soft tube will be placed in the operating room through the nose, down the esophagus, into the stomach. This tube will be used to give feedings while the esophagus heals. The feeding tube will be removed after the esophagus is healed and full oral feedings are established. If repair of the esophagus is delayed, because of a wide gap between the pouches, a gastrostomy tube will be placed in the stomach, at the time the tracheoesophageal fistula is closed. The gastrostomy tube will be used to give feedings and to remove (decompress) air from the stomach until the final repair of the esophagus is performed. The gastronomy tube will remain in place as long as your child requires this method of feeding.
Intravenous fluids will be given until breast milk or formula feedings can be started. Feedings are begun once your baby has recovered from the operation, usually after several days. Feedings will be given one of two ways. If the esophagus is repaired primarily, a thin soft tube will be placed in the operating room through the nose, down the esophagus, into the stomach. This tube will be used to give feedings while the esophagus heals. The feeding tube will be removed after the esophagus is healed and full oral feedings are established. If repair of the esophagus is delayed, because of a wide gap between the pouches, a gastrostomy tube will be placed in the stomach, at the time the tracheoesophageal fistula is closed. The gastrostomy tube will be used to give feedings and to remove (decompress) air from the stomach until the final repair of the esophagus is performed. The gastronomy tube will remain in place as long as your child requires this method of feeding.
How long will my child be in the hospital?
Your baby will remain in the Intensive Care Nursery until he/ she is taking full feedings by orally, or gastrostomy tube, and is gaining weight. This usually takes several weeks. Babies born with esophageal atresia and tracheoesophageal fistula may have tracheomalacia (soft airways). This occurs during pregnancy as a result of compression of the dilated upper pouch of the esophagus on the developing trachea. Tracheomalacia may contribute to breathing problems after birth and after hospital discharge. Tracheomalacia is a condition the baby usually outgrows as the airways become firmer.
Babies with esophageal atresia and tracheoesophageal fistula also have gastroesphageal reflux, a back flow of contents from the stomach into the esophagus. This is due to poor motility, or contractility, of the lower portion of the esophagus. Reflux may contribute to irritation of the esophagus and cause pain. The irritating effects of the stomach contents on the esophagus may cause tightening (stricture) at the surgical site in the esophagus. To prevent this problem, your baby will be started on an antacid medication and a medication to enhance stomach emptying. These medications will be continued after hospital discharge, with dosages adjusted as your child gains weight.
If your baby has a gastrostomy tube, the nurses will show you how to care for it and use it to administer feeding or decompress air from the stomach. A replacement gastrostomy tube of the same size will be sent home with you at discharge. Feeding supplies will be ordered for you by the Discharge Coordinator in the Intensive Care Nursery. These supplies will be delivered to your home by a home care company. Nurses will be requested to visit you and your child after discharge to help ease the transition from the hospital to home.
When do I see the surgeon after the hospital discharge?
If all is going well, a visit to our office at a specific time is not required. A visit to your child's Primary Provider, at one to two weeks after the discharge, is recommended. Children with esophageal atresia and tracheoesophageal fistula may develop esophageal narrowing (stricture) at the site of repair. If this occurs, your child will have trouble swallowing liquids or solids. If the problem is severe you may notice your child coughing or choking on food, vomiting, or refusing to take food or liquids. If you suspect there is a stricture call our office as soon as possible. We will arrange for a special x-ray called an esophagram, which will help identify any narrowing or stricture of the esophagus. Surgical dilation (stretching) of the esophageal stricture may be required and will be performed under anesthesia.
Children with esophageal atresia can have longterm respiratory difficulties as well as feeding problems and slow growth. We have a program for children withesophageal atresia called the Life Clinic. In this program, we closely monitor children with esophageal atresia in conjunction with problems in nutrition, feeding therapy, pulmonary, and gastroenterology. We will make an appointment for your child in our Life Clinic at the time of hospital discharge.
Homecare
Your baby will remain in the Intensive Care Nursery until he/ she is taking full feedings by mouth, or gastrostomy tube, and is gaining weight. This usually takes several weeks. Once discharged, babies may have problems with acid reflux for the first year. If your baby has a gastrostomy tube, the nurses will show you how to care for it and use it to administer feeding or decompress air from the stomach.
Acid Reflux Treatment
Babies with esophageal atresia and tracheoesophageal fistula also have gastroesphageal reflux, a back flow of contents from the stomach into the esophagus. To prevent this irritation, your baby will be started on an antacid medication and a medication to enhance stomach emptying. These medications are continued after hospital discharge for as long as needed, with dosages adjusted by your peditrician as your child gains weight. Please do not stop these medications without consulting your child's surgeon.
Care for a Gastrostomy Tube
Your nurses will instruct you how to care for the gastrostomy tube. At discharge, a replacement gastrostomy tube of the same size will be sent home with you. Feeding supplies will be ordered for you by the Discharge Coordinator in the Intensive Care Nursery. These supplies will be delivered to your home by a homecare company. Nurses will be requested to visit you and your child after discharge to help ease the transition from the hospital to home.
For more info read Homecare Guidelines for Gastrostomy Tubes
Do I see the surgeon again after the hospital discharge?
If all is going well, a visit to our office at a specific time is not required. A visit to your child's Primary Provider, at one to two weeks after the discharge, is recommended. Children with esophageal atresia and tracheoesophageal fistula may develop esophageal narrowing (stricture) at the site of repair. If this occurs, your child will have trouble swallowing liquids or solids. If the problem is severe you may notice your child coughing or choking on food, vomiting, or refusing to take food or liquids. If you suspect there is a stricture call our office as soon as possible. We will arrange for a special x-ray called an esophagram, which will help identify any narrowing or stricture of the esophagus. Surgical dilation (stretching) of the esophageal stricture may be required and will be performed under anesthesia.
When do I call the surgeon's office?
Call our office at 415-476-2538 for the following:
- Any concerns you have about your child's recovery
- A temperature of 101°F or higher
- A red incision
- Increasing pain and tenderness at the incision
- Any liquid coming out of the incision
- Difficulty swallowing liquids or solids
- Questions regarding the gastrostomy tube
- Chronic lung problems should be addressed with a pulmenologist
Parent support organizations
EA/TEF Child and Family Support Connection, Inc.
111 W. Jackson Blvd., Suite 1145
Chicago, Ill. 60604-3502
Phone: 312-987-9085
Email: [email protected]
Web: www.eatef.org
