Type 1 Diabetes
Diabetes is a serious disease, which, if not controlled, can be life threatening. It is often associated with long-term complications that can affect every system and part of the body. Diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, amputation, and nerve damage. It can affect pregnancy and cause birth defects, as well
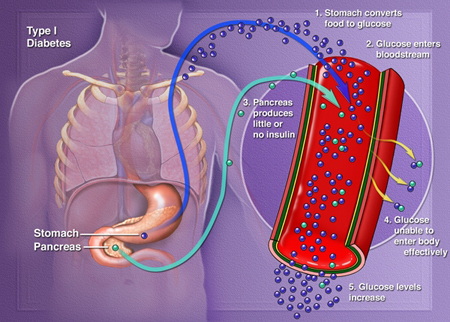
Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Damage to beta cells results in an absence or insufficient production of insulin produced by the body. Type 1 diabetes an autoimmune disease in which the body views the beta cells (insulin producing cells found in the islets of the pancreas) as a foreign substance, so the patient's immune system attacks the islets and kills them. Since insulin is necessary to sustain life, the missing insulin has to be replaced. The replacement insulin is administered by injection using a syringe or an insulin pump, which delivers the insulin under the skin.
It is estimated that 5-10% of Americans who are diagnosed with diabetes have type 1 diabetes. Most people with type 1 diabetes do not have a family history of the disease. We do not know how to prevent the onset of type 1 diabetes.
 |
|
| Image courtesy of Clinical Islet Transplantation (CIT) Consortium, sponsored by National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK) and National Institute of Allergy and Infectious Diseases (NIAID) |
Treatments for Type 1 Diabetes
Intensive Insulin Therapy
There are many different insulins for many different situations and lifestyles, and there are more than 20 types of insulin sold in the United States. These insulins differ in how they are made, how they work in the body, and price. A molecule that is identical to human insulin can be manufactured. In addition, insulin can be obtained from pigs, as people will respond to pig insulin. Future availability of animal insulin is uncertain.
Insulin may be taken by means of a shot (often several times a day), or infused through catheter (a small needle) attached to an insulin pump. Recently an inhalable insulin has been approved by the FDA.
It is important for anyone with diabetes to be careful about the type, timing and amount of food they eat. People with diabetes also need to monitor their bloodsugars carefully through frequent finger prick glucose testing. A person with diabetes may experience long term complications if tight blood sugar control is not maintained; likewise, control that is too tight may result in severe hypoglycemic (low blood sugar) reactions.
Pancreas Transplant
The first pancreas transplant was performed in 1966. Long-term success has steadily improved and the risks have decreased. Whole organ pancreas transplant is a major operation and can be associated with complications, such as bleeding, infection, inflammation of the pancreas and clots in the blood vessels around the pancreas. It is most often performed when a patient also needs a kidney transplant. The success rate (long-term insulin independence) with pancreas transplantation was initially low, but increased dramatically in the 1980s. After one year about 85% of pancreas transplant recipients are insulin independent. By the 1990s, more than 1000 pancreas transplants a year were being done worldwide, the majority in the U.S.
Islet Transplantation
Islet transplantation is still in the experimental stages. The advantages over pancreas transplantation are that it does not require a major operation and the procedure has a small complication rate. Nevertheless, islet transplantation can be associated with bleeding, clotting of blood vessels in the liver, or damage to the gall bladder. At this time, the results are not as good as pancreas transplantation.
Lastly, it is important to note that individuals that receive a pancreas or islet transplant must take immunosuppressive medications as long as the pancreas or islets are functioning.
