Minimally Invasive Atrial Septal Defect (ASD) Closure
|
An atrial septal defect (ASD) is a congenital heart defect where there is a hole in the atrial septum, the wall which separates the right and left atria. A small opening between the two atria (foramen ovale) is always present at birth, but usually seals off shortly thereafter. If the natural opening persists, it is called patent foramen ovale, if the opening is bigger than that and involves a defect in the muscular septum, it is called ASD. Each year about 1,966 babies in the United States are born with an ASD. Girls are twice as often affected than boys.
What symptoms can an ASD cause?
Symptoms can develop in childhood or later in life, depending on the size of the defect. Some may experience shortness of breath, fatigue, heart palpitations, or a decrease in exercise capacity. Patients usually have an audible heart murmur that is caused by the extra blood flow across the pulmonary valve to the lungs.
Why is an ASD potentially dangerous?
Patients with a big ASD are more likely to develop congestive heart failure or stroke. Because of the excessive flow of blood into the right atrium, right ventricle and lungs, this enlarges the right atrium and right ventricle and increases pressures in the pulmonary artery. An enlarged right atrium can cause arrhythmias. The lung vessels can become stiff and increase the resistance of the pulmonary circulation and result in a so-called Eisenmenger syndrome. Such patients are very sick, acquire a blue tinge to the skin, and are in heart failure.
When should an ASD be treated?
A significant ASD should always be treated, regardless of the age of the patient. Some of the structural changes in the heart caused by an ASD over time are not entirely reversible. ASD closure before irreversible changes occur is therefore recommended. Most patients, children as well as adults, usually experience marked improvement of their symptoms after ASD closure.
How can an ASD be closed?
Surgical Closure
Patients are supported by a heart-lung machine intraoperatively and the ASD is approached through an opening in the right atrium
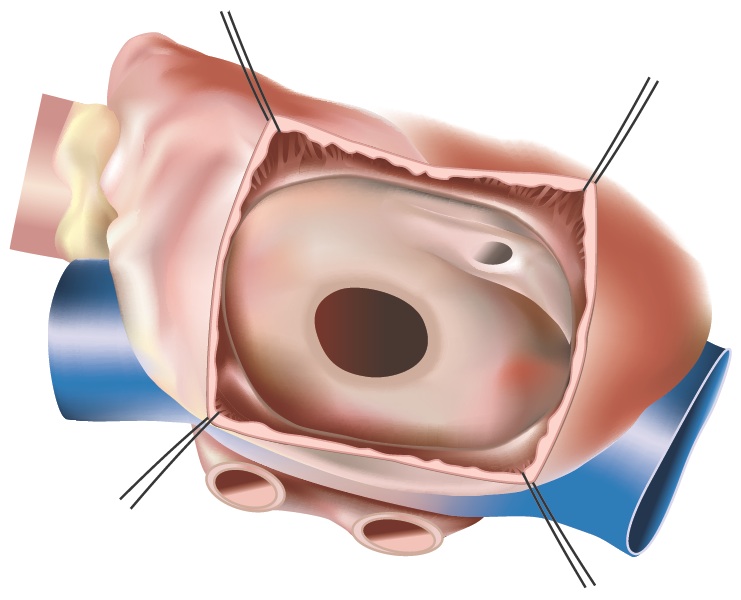
Figure 1 - Open ASD
Smaller ASDs can simply be closed using a suture and oversewing the hole. For larger ASDs, a patch is usually used to close the hole. This patch can be taken from the pericardium (the sac that surrounds the heart) or from synthetic materials such as Dacron or Teflon.
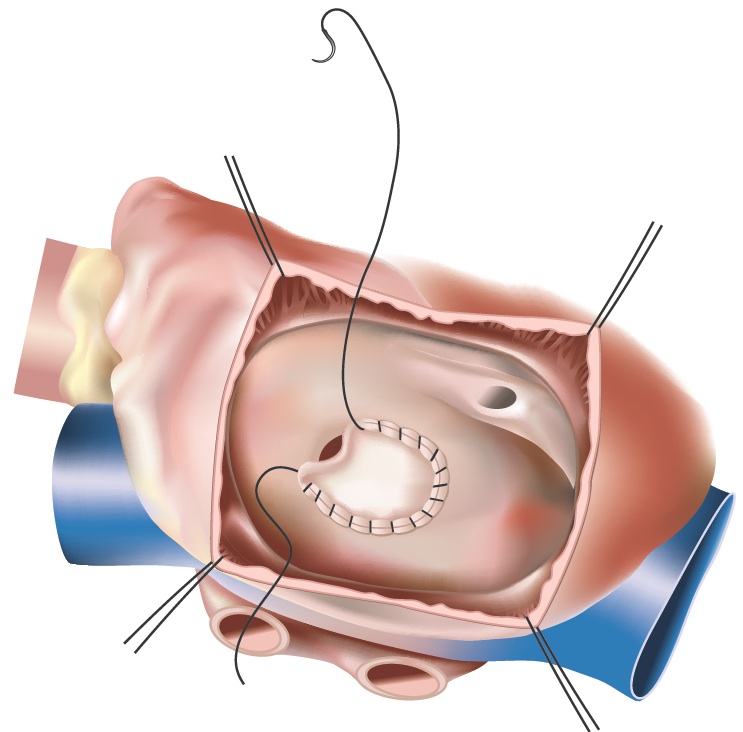
Figure 2 - Closed ASD
Can surgery be done using keyhole incisions?
Most patients with an ASD are candidates for minimally invasive surgery. Surgeons perform the operation by making only a small 4-6 cm incision on the right side of the chest instead of the large midline-incision and division of the sternum used in traditional open surgery.
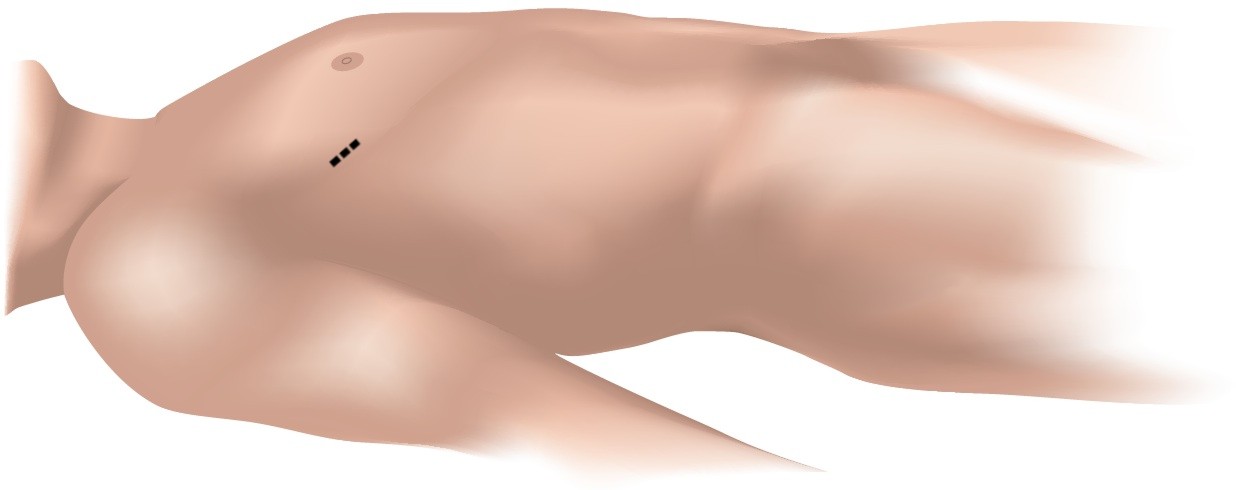
Fig. 3 - Incision
The surgery is performed through the small space between the ribs. The heart-lung machine is inserted via a small incision in the groin, allowing the heart to be stopped for the sewing of the patch. A soft retractor is inserted, which gently opens the narrow space between the ribs, enabling the surgeon to insert the specialized minimally invasive instruments. An endoscope, ideally with a 3D camera, is inserted that will provide a high-resolution image of the heart and the ASD.
Using this technique, the stability of the chest is fully preserved, patients recover more quickly, and the minimal scar will be barely visible after the patient recovers.
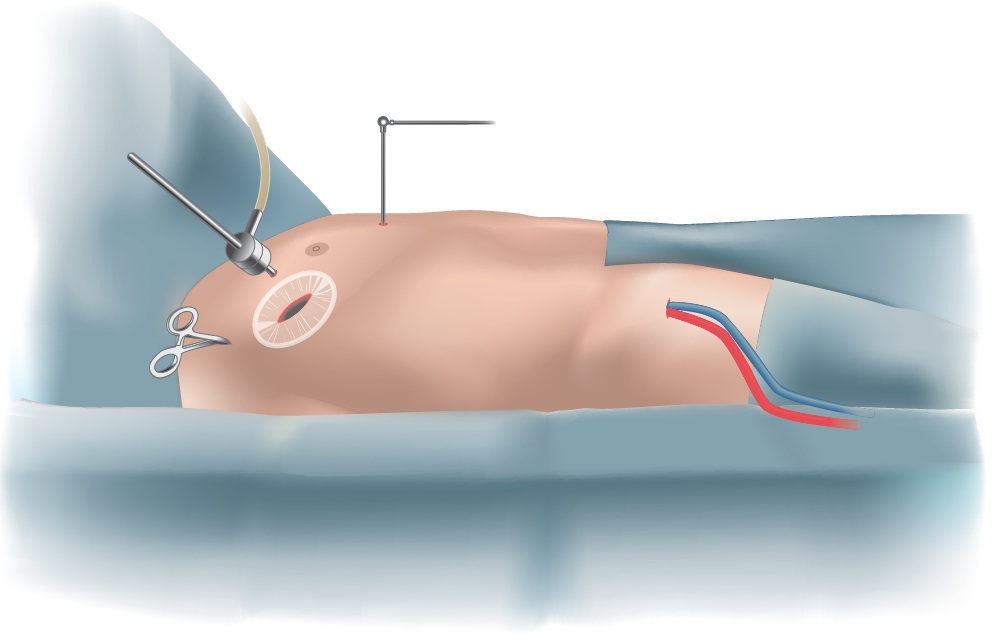
Fig. 4 - Surgical setup
Are there alternative options?
If the ASD is not too large and has a sufficient rim all around, a closure devices may be introduced into the heart with the use of a catheter. The catheter enters from the groin, continues into the heart, and goes across the ASD to deploy the device.

 "UCSF offers a minimally invasive approaches for Atrial Septal Defect (ASD) Closure. The operation is performed using a small 4-6 cm incision through the small space between the ribs. The
"UCSF offers a minimally invasive approaches for Atrial Septal Defect (ASD) Closure. The operation is performed using a small 4-6 cm incision through the small space between the ribs. The