Diabetic Peripheral Neuropathy
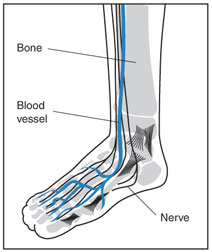
Diabetic peripheral neuropathy is a condition in which the nerves of the arms, hands, legs and feet become damaged by diabetes. Peripheral neuropathy can lead to numbness, loss of sensation, and sometimes pain. It is the most frequent complication of diabetes, eventually impacting 60% to 70% of persons with the disease.
Diabetic peripheral neuropathy develops slowly and insidiously, worsening over time. Signs of the disease may be present even before a person is formally diagnosed with diabetes. Symptoms begin in the longest nerves in the body, affecting the feet first and later the hands in a “stocking-glove” pattern. The symptoms usually spread slowly and evenly up the legs and arms.
Diabetes also causes inflammation of the blood vessel walls and atherosclerosis, or hardening of the arteries, leading to poor blood circulation in the lower extremities and development of peripheral artery disease (PAD). The lack of blood flow and constricted arteries also impair the body's ability to fight infection. Between 20-30% of people with diabetes also have PAD.
Causes
In diabetic peripheral neuropathy, chronically high blood sugar levels as a result of diabetes damage nerves not only in the extremities, but throughout the body. This impairs nerve signaling between the brain, and vital organs and tissues of the body. Three groups of nerves are affected by diabetic peripheral neuropathy:
Sensory Nerves
 Sensory nerves enable people to feel pain, temperature, and other sensations. When the sensory nerves are damaged, a person with diabetes might not feel heat, cold, or pain. A cut or sore on a foot, a burn from hot water, or exposure to extreme cold causing frostbite might go completely unnoticed. The sore or exposed area may then become infected, causing a foot ulcer, which may then not heal due to the body's impaired ability to fight infection.
Sensory nerves enable people to feel pain, temperature, and other sensations. When the sensory nerves are damaged, a person with diabetes might not feel heat, cold, or pain. A cut or sore on a foot, a burn from hot water, or exposure to extreme cold causing frostbite might go completely unnoticed. The sore or exposed area may then become infected, causing a foot ulcer, which may then not heal due to the body's impaired ability to fight infection.
The perception of sensory nerve damage can vary by individual. Some people may feel tingling, then later feel pain. Others have numbness and lose the feeling in their fingers and toes. Since these changes happen slowly and gradually, they may go unnoticed. And because the changes are subtle and occur over years or even decades, the signs of nerve damage may end up being ignored and attributed to simply aging.
Motor Nerves
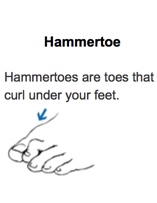
Motor nerves control muscles and give them their strength and tone. Peripheral neuropathy may also cause muscle weakness and loss of reflexes, especially at the ankle, leading to changes in the way a person walks. Foot deformities, such as bunions and hammertoes, may occur, as well as collapse of the midfoot, a condition known as Charcot foot.
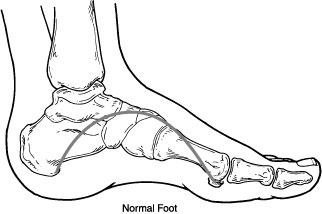
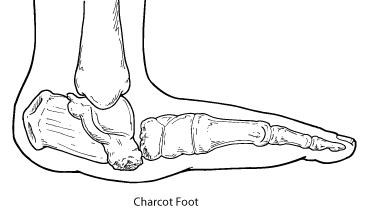
In Charcot foot, the joints in the foot collapse and the foot eventually becomes deformed
The loss of foot structure may also cause shoes to rub against toes, causing sores. Blisters and sores may appear on numb areas of the foot because an injury goes unnoticed. If an infection occurs and is not treated promptly, the infection may spread to the bone, a condition known as osteomyelitis, and the foot may have to be amputated. Many amputations are preventable if minor problems are caught and treated in time.
 |
 |
 |
Autonomic Nerves
Autonomic nerves enable the body to perform involuntary functions, such as sweating. When these nerves are damaged, the skin on the foot can dry out and crack. Breaks in the skin, lack of sensory awareness, and/or motor neuropathy can result in the development of a diabetic foot ulcer.
Symptoms
Symptoms of diabetic peripheral neuropathy include:
Sensory Neuropathy
- Inability to feel pain, temperature changes, and changes in pressure
- Numbness or tingling in the feet
- Pain or discomfort in the lower extremities including:
- Prickly, sharp pain
- Burning feet
- Pinching
- Pins and needles
- Exaggerated sensitivity to touch
Motor Neuropathy
- Muscle weakness and loss of muscle tone in the feet or legs
- Loss of balance
- Changes in the shape or structure of the foot leading to areas of increased pressure
Autonomic Neuropathy
- Dry feet caused by damage to the nerves controlling the sweat glands
- Cracks in the skin of the foot
Diagnosis
Peripheral neuropathy is diagnosed based on objective signs, symptoms, and a physical exam that includes a check of blood pressure, heart rate, muscle strength, reflexes, and sensitivity to position changes, vibration, temperature, or light touch.
Foot Exam
A comprehensive foot exam will assess the skin, muscles, bones, circulation, and sensation of the feet. This includes evaluating the protective sensation or feeling in the feet by touching them with a nylon monofilament—similar to a bristle on a hairbrush—attached to a wand, or by pricking them with a pin.
People that are unable to sense pressure from a pinprick or monofilament have lost protective sensation and are at risk for developing foot sores and ulcers that may not heal properly. Temperature perception may also be checked with a tuning fork, which is more precise than touch pressure in assessing vibration perception.
Other Tests
- Nerve conduction studies or electromyography are sometimes used to help determine the type and extent of nerve damage. Nerve conduction studies check the transmission of electrical current through a nerve. Electromyography shows how well muscles respond to electrical signals transmitted by nearby nerves. These tests are rarely needed to diagnose neuropathy.
- A check of heart rate variability shows how the heart responds to deep breathing and to changes in blood pressure and posture.
- Ultrasound uses sound waves to produce an image of internal organs. An ultrasound of the bladder and other parts of the urinary tract, for example, can be used to assess the structure of these organs and show whether the bladder empties completely after urination.
Treatment
Blood Glucose Control
The first treatment step is to bring blood glucose levels within the normal range to help prevent further nerve damage. Blood glucose monitoring, meal planning, physical activity, and diabetes medicines or insulin will help control blood glucose levels. Symptoms may get worse when blood glucose is first brought under control, but over time, maintaining lower blood glucose levels helps lessen symptoms. Good blood glucose control may also help prevent or delay the onset of further problems. As scientists learn more about the underlying causes of neuropathy, new treatments may become available to help slow, prevent, or even reverse nerve damage.
Pain Relief
Painful diabetic neuropathy is usually treated with oral medications which include:
- Tricyclic antidepressants, such as amitriptyline, imipramine, and desipramine (Norpramin, Pertofrane)
- Other types of antidepressants, such as duloxetine (Cymbalta), venlafaxine, bupropion (Wellbutrin), paroxetine (Paxil), and citalopram (Celexa)
- Anticonvulsants, such as pregabalin (Lyrica), gabapentin (Gabarone, Neurontin), carbamazepine, and lamotrigine (Lamictal)
- Opioids and opioidlike drugs, such as controlled-release oxycodone, an opioid; and tramadol (Ultram), an opioid that also acts as an antidepressant
Duloxetine and pregabalin are approved by the U.S. Food and Drug Administration specifically for treating painful diabetic peripheral neuropathy.
Treatments that are applied to the skin—typically to the feet—include capsaicin cream and lidocaine patches (Lidoderm, Lidopain). Studies suggest that nitrate sprays or patches for the feet may relieve pain. Studies of alpha-lipoic acid, an antioxidant, and evening primrose oil suggest they may help relieve symptoms and improve nerve function in some patients.
A device called a bed cradle can keep sheets and blankets from touching sensitive feet and legs. Acupuncture, biofeedback, or physical therapy may help relieve pain in some people. Treatments that involve electrical nerve stimulation, magnetic therapy, and laser or light therapy may be helpful but need further study. Researchers are also studying several new therapies in clinical trials.
Physical Therapy
The patient may also be offered physical therapy to help reduce balance problems or other symptoms.
