Hyperthyroidism
Hyperthyroidism is a disorder that occurs when the thyroid gland makes more thyroid hormone than the body needs. It is sometimes called thyrotoxicosis, the technical term for too much thyroid hormone in the blood. About 1 percent of the U.S. population has hyperthyroidism. Women are much more likely to develop hyperthyroidism than men.
The thyroid gland's production of thyroid hormones (T3 and T4) is triggered by thyroid-stimulating hormone (TSH), which is made by the pituitary gland.
What is the thyroid gland?
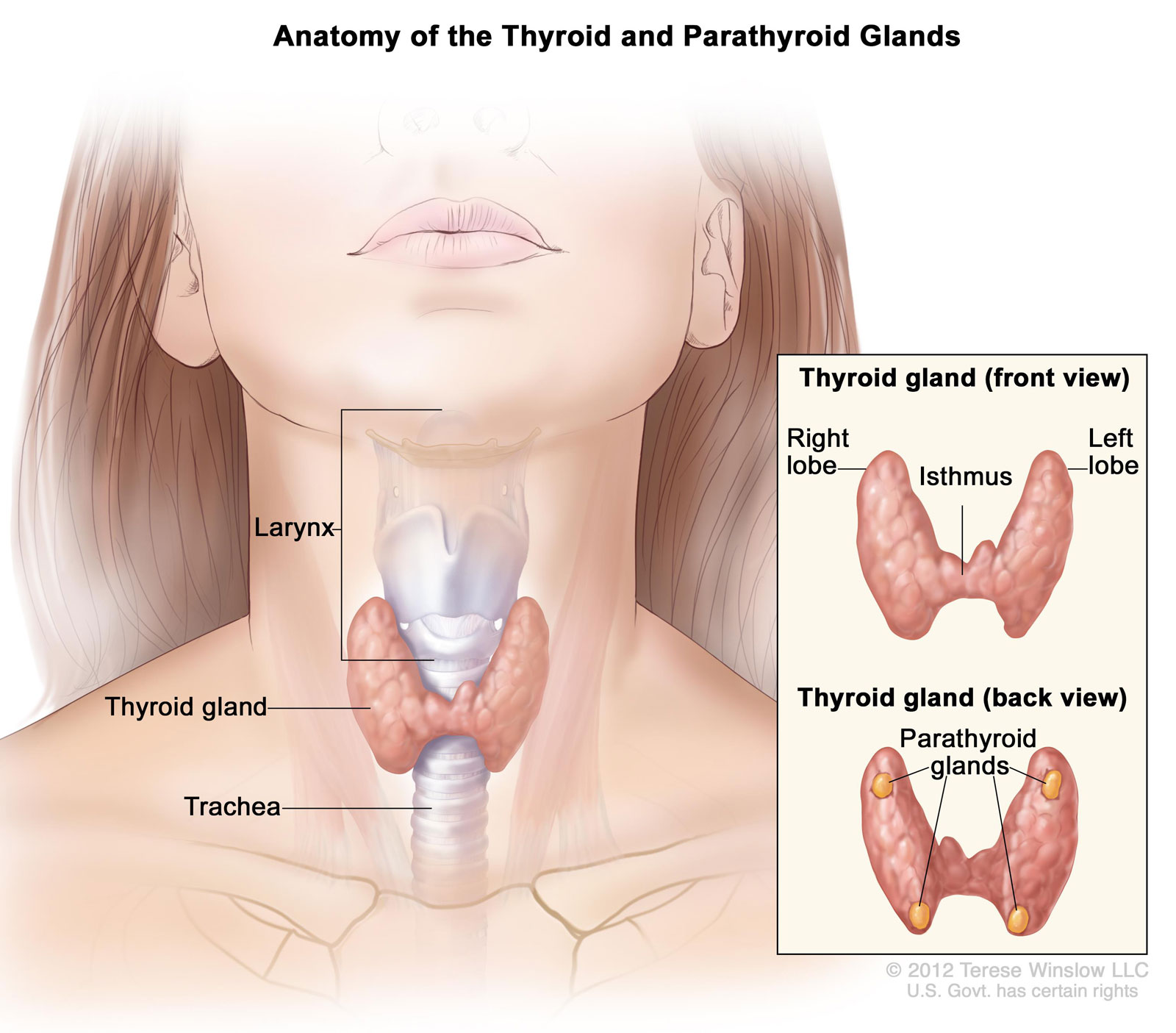
The thyroid is a 2-inch-long, butterfly-shaped gland weighing less than an ounce. Located in the front of the neck below the larynx, or voice box, it is composed of two lobes, one on each side of the windpipe.
The thyroid is one of the glands that make up the endocrine system. The endocrine glands produce, store, and release hormones into the bloodstream that travel through the body and direct the activity of the body's cells. Thyroid hormones regulate metabolism-the way the body uses energy-and affect nearly every organ in the body.
Hormones Made by the Thyroid Gland
The thyroid gland makes two thyroid hormones, triiodothyronine (T3) and thyroxine (T4). Thyroid hormones affect metabolism, brain development, breathing, heart and nervous system functions, body temperature, muscle strength, skin dryness, menstrual cycles, weight, and cholesterol levels.
A third hormone produced by the thyroid gland, calcitonin, is not considered a thyroid hormone as such, but affects calcium levels in the blood and controls the buildup of calcium in the bones.
Thyroid hormone production is regulated by thyroid-stimulating hormone (TSH), which is made by another gland in the endocrine system called the pituitary, located in the brain.
What causes hyperthyroidism?
Hyperthyroidism has several causes, including
- Graves' disease
- one or more thyroid nodules
- thyroiditis, or inflammation of the thyroid gland
- ingesting too much iodine
- overmedicating with synthetic thyroid hormone, which is used to treat underactive thyroid
Rarely, hyperthyroidism is caused by a pituitary adenoma, which is a noncancerous tumor of the pituitary gland. In this case, hyperthyroidism is due to too much TSH.
Graves' Disease
Graves' disease, also known as toxic diffuse goiter, is the most common cause of hyperthyroidism in the United States. Graves' disease is an autoimmune disease, which means the body's immune system acts against its own healthy cells and tissues. In Graves' disease, the immune system makes an antibody called thyroid stimulating immunoglobulin (TSI), which mimics TSH and causes the thyroid to make too much thyroid hormone.
Thyroid Nodules
Thyroid nodules, also called adenomas, are lumps in the thyroid. Thyroid nodules are common and usually noncancerous. About 3 to 7 percent of the population has them. However, nodules may become overactive and produce too much hormone. A single overactive nodule is called a toxic adenoma.
When multiple nodules are overactive, the condition is called toxic multinodular goiter. Often found in older adults, toxic multinodular goiter can produce a large amount of excess thyroid hormone.
Thyroiditis
Several types of thyroiditis can cause hyperthyroidism. Thyroiditis does not cause the thyroid to produce excess hormone. Instead, it causes stored thyroid hormone to leak out of the inflamed gland and raise hormone levels in the blood.
Subacute thyroiditis. This condition involves painful inflammation and enlargement of the thyroid gland. Doctors aren't sure what causes subacute thyroiditis, but it may be related to a viral or bacterial infection. The condition usually goes away on its own in a few months. Many people with subacute thyroiditis briefly develop hypothyroidism-when hormone levels are too low-after the hyperthyroidism resolves but before the thyroid gland is completely healed.
Postpartum thyroiditis. About 8 percent of women who have been pregnant develop postpartum thyroiditis within a few months of giving birth. Postpartum thyroiditis is believed to be an autoimmune condition and causes hyperthyroidism that usually lasts for 1 to 2 months. The condition is likely to recur with future pregnancies. As with subacute thyroiditis, women with postpartum thyroiditis often develop hypothyroidism before the thyroid gland is completely healed. In some women, the gland does not heal and hormone levels remain low. These women must take thyroid hormone replacement for the rest of their lives.
Silent thyroiditis. This type of thyroiditis is called "silent" because it is painless, as is postpartum thyroiditis, even though the thyroid may be enlarged. Like postpartum thyroiditis, silent thyroiditis is probably an autoimmune condition and sometimes develops into permanent hypothyroidism.
Iodine Ingestion
The thyroid gland uses iodine to make thyroid hormone, so the amount of iodine you consume influences the amount of thyroid hormone your thyroid makes. In some people, consuming large amounts of iodine may cause the thyroid to make excess thyroid hormone. Sometimes significant amounts of iodine are contained in medications-such as amiodarone, which is used to treat heart problems-or in supplements containing seaweed. Some cough syrups also contain large amounts of iodine.
Overmedicating with Thyroid Hormone
Some people who take thyroid hormone for hypothyroidism may take too much. If you take synthetic thyroid hormone, see your doctor at least once a year to have your thyroid hormone levels checked and follow your doctor's instructions about the dose you take. Some medications may also interact with your synthetic thyroid hormone to raise levels in your blood. Ask your health care professional about drug interactions when starting new medications.
What are the symptoms of hyperthyroidism?
Hyperthyroidism has many symptoms that can vary from person to person. Some common symptoms of hyperthyroidism are
- nervousness or irritability
- fatigue or muscle weakness
- trouble sleeping
- heat intolerance
- hand tremors
- rapid and irregular heartbeat
- frequent bowel movements or diarrhea
- weight loss
- mood swings
- goiter, which is an enlarged thyroid that may cause your neck to look swollen
Who is likely to develop hyperthyroidism?
Women are five to 10 times more likely than men to develop hyperthyroidism. The American Thyroid Association recommends that adults, particularly women, have a blood test to detect thyroid problems every 5 years starting at age 35.
Certain factors can increase your chances of developing thyroid disorders. You may need more frequent testing if you
- have had a thyroid problem before, such as goiter or thyroid surgery
- have pernicious anemia; type 1 diabetes; or primary adrenal insufficiency, a hormonal disorder
- have a family history of thyroid disease
- eat large amounts of food containing iodine, such as kelp, or use iodine-containing medications such as amiodarone, a heart medication
- are older than 60 years
- have been pregnant or delivered a baby within the past 6 months
Getting tested routinely helps uncover thyroid problems-especially subclinical problems. Subclinical means that a person has no apparent symptoms. Some doctors treat subclinical hyperthyroidism immediately; others prefer to leave it untreated but monitor their patients for signs that the condition is worsening.
Hyperthyroidism in the Aging Population
Hyperthyroidism is more common in people over age 60 and is often caused by thyroid nodules. Hyperthyroidism in this age group is sometimes misdiagnosed as depression or dementia because older adults do not always display the more common symptoms of the disorder. For example, older adults may lose their appetites, whereas younger people tend to have increased appetites. Older adults with hyperthyroidism may seem disinterested or withdraw socially. They may have different physical symptoms as well.
Treating subclinical hyperthyroidism may be more important in older adults than in younger patients. For people over age 60, subclinical hyperthyroidism increases the chance of developing a rapid, irregular heartbeat, known as atrial fibrillation-a condition that may lead to heart failure or stroke. Untreated hyperthyroidism can also speed the bone-thinning disease osteoporosis, particularly in women, and increase the likelihood of bone fractures.
Pregnancy and Hyperthyroidism
If you have hyperthyroidism, you should discuss your condition with your doctor before becoming pregnant. Uncontrolled hyperthyroidism raises your chance of miscarriage, preterm delivery, and preeclampsia, a potentially serious complication that increases blood pressure.
Symptoms of hyperthyroidism may be difficult to assess during pregnancy. Normally, the thyroid gland gets bigger in healthy women when they become pregnant. That normal enlargement, combined with fatigue, makes a new thyroid problem easy to miss. A rapid heart rate and unexplained weight loss or failure to have normal pregnancy weight gain are signs that hyperthyroidism could be developing.
Diagnosis
Your doctor will begin by asking you about your symptoms and performing a thorough physical examination. Your doctor may then use several tests to confirm a diagnosis of hyperthyroidism and to find its cause.
Thyroid-Stimulating Hormone (TSH) Test
The ultrasensitive TSH test will probably be the first test your doctor performs. This test can detect even tiny amounts of TSH in the blood and is the most accurate measure of thyroid activity available. The TSH test is especially useful in detecting mild hyperthyroidism.
The TSH test is based on the way TSH and thyroid hormone work together. The pituitary gland boosts TSH production when the thyroid is not making enough thyroid hormone; the thyroid normally responds by making more hormone. Then, when the body has enough thyroid hormone circulating in the blood, TSH output drops. In people who produce too much thyroid hormone, the pituitary shuts down TSH production, leading to low or even undetectable TSH levels in the blood.
Generally, a TSH reading below normal indicates hyperthyroidism and a reading above normal means a person has hypothyroidism.
Other Tests
If your doctor confirms you have hyperthyroidism, additional tests may be needed to find the cause and determine the best treatment.
T3 and T4 test. This test will show the levels of T3 and T4 in your blood. If you have hyperthyroidism, the levels of one or both of these hormones in your blood will be higher than normal.
Thyroid-stimulating immunoglobulin (TSI) test. This test, also called a thyroid-stimulating antibody test, measures the level of TSI in your blood. Most people with Graves' disease have this antibody, but people whose hyperthyroidism is caused by something else do not.
Radioactive iodine uptake test. The radioactive iodine uptake test measures the amount of iodine your thyroid collects from the bloodstream. Measuring the amount of iodine in your thyroid will help your doctor know what is causing your hyperthyroidism. For example, low levels of iodine uptake might be a sign of thyroiditis, whereas high levels could indicate Graves' disease.
Thyroid scan. A thyroid scan shows how and where iodine is distributed in your thyroid. This information helps your doctor diagnose the cause of your hyperthyroidism by providing images of nodules and other possible thyroid irregularities.
Treatment
Treatment depends on the cause of hyperthyroidism and how severe it is. When choosing a treatment, doctors consider a patient's age, possible allergies to or side effects of the medications, other conditions such as pregnancy or heart disease, and the availability of an experienced thyroid surgeon.
The aim of treatment is to bring thyroid hormone levels to a normal state, thus preventing long-term complications, and to relieve uncomfortable symptoms. No single treatment works for everyone. The three treatment options are medications, radioiodine therapy, and surgery.
Medications
Your doctor may prescribe a drug called a beta blocker to reduce your symptoms until other treatments take effect. Beta blockers act quickly to relieve many of the symptoms of hyperthyroidism, such as tremors, rapid heartbeat, and nervousness. Most people feel better within hours of taking these drugs. Beta blockers act by blocking the effects of thyroid hormone on your body, but they do not stop thyroid hormone production.
Antithyroid drugs interfere with thyroid hormone production by blocking the way the thyroid gland uses iodine to make thyroid hormone. In the United States, doctors prescribe methimazole (Tapazole) and propylthiouracil (PTU) for most types of hyperthyroidism. Antithyroid drugs are not used to treat thyroiditis.
Once you begin treatment with antithyroid drugs, your thyroid hormone levels may not move into the normal range for several weeks or months. The average treatment time is about 1 to 2 years, but treatment can continue for many years. Antithyroid therapy is the easiest way to treat hyperthyroidism but often does not produce permanent results.
Antithyroid drugs can cause side effects in some people. Side effects may include
- allergic reactions such as rashes and itching
- a decrease in the number of white blood cells in the body, which can lower a person's resistance to infection
- liver failure, in rare cases
If you develop a skin rash, yellowing of your eyes or skin, persistent sore throat, or fever while taking antithyroid drugs, call your doctor right away.
Pregnant women should not take methimazole and should be monitored if they take PTU. Women who are breastfeeding should take only very small doses of either drug.
Radioiodine Therapy
Radioactive iodine-131 is a common and effective treatment for hyperthyroidism. Because your thyroid gland collects iodine to make thyroid hormone, it will collect the radioactive iodine in the same way. The radioactive iodine will gradually destroy the cells that make up the thyroid gland but will not affect other tissues in the body.
Sometimes more than one round of radioiodine therapy is needed to bring thyroid hormone production into the normal range. In the meantime, treatment with beta blockers can control your symptoms.
Although iodine-131 is not known to cause birth defects or infertility, radioiodine therapy is not used in pregnant women or women who are breastfeeding. Radioactive iodine can be harmful to the fetus' thyroid, and it can be passed from mother to child in breast milk.
Almost everyone who receives radioactive iodine treatment eventually develops hypothyroidism. But doctors consider this an acceptable outcome, since hypothyroidism is easier to treat and has fewer long-term complications than hyperthyroidism. If you develop hypothyroidism, you will have to take some type of synthetic thyroid hormone replacement.
Thyroid Surgery
The least-used treatment is surgery to remove part or most of the thyroid gland. Doctors sometimes choose surgery to treat pregnant women who cannot tolerate antithyroid drugs, people with very large goiters, or people who have cancerous thyroid nodules. Keep in mind that hyperthyroidism does not cause cancer.
Before surgery, your doctor may temporarily bring your thyroid hormone levels into the normal range with antithyroid drugs. This presurgical treatment prevents a condition called thyroid storm-a sudden, severe worsening of symptoms-that can occur when hyperthyroid patients have general anesthesia.
A few days before your scheduled surgery, your doctor may give you nonradioactive iodine drops, such as Lugol's iodine or supersaturated potassium iodide. This extra iodine will help reduce blood supply to the thyroid gland and make your surgery safer.
When part of the thyroid is removed-as a treatment for toxic nodules, for example-your thyroid hormone levels may return to normal. But some surgical patients may still develop hypothyroidism and need to take synthetic thyroid hormone. If your entire thyroid is removed, you will need lifelong thyroid hormone replacement. After surgery, your doctor will continue to monitor your thyroid hormone levels.
Although uncommon, certain problems can occur in thyroid surgery. Your parathyroid glands could be damaged because they are located very close to your thyroid gland. These glands help control calcium levels in your body. Damage to the laryngeal nerve, also located close to the thyroid gland, could lead to voice changes or breathing problems. When surgery is performed by an experienced surgeon, less than 1 percent of patients have permanent complications.
