Thyroidectomy
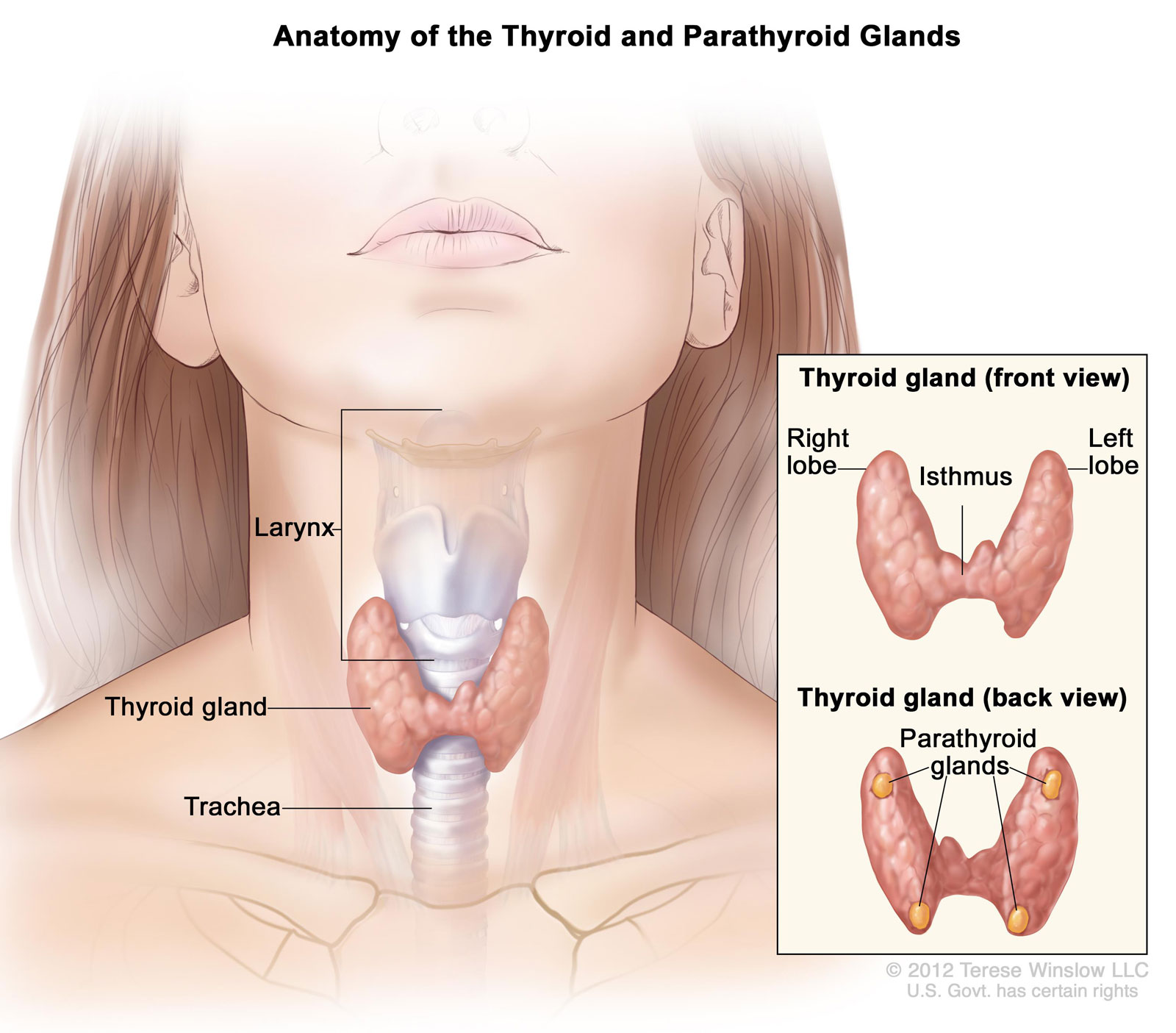
The thyroid gland is a butterfly-shaped organ composed of two cone-like lobes or wings connected via the isthmus. The gland regulates metabolism by secreting hormones. When diseases affect the thyroid, its size or activity may become abnormal.
What is a Thyroidectomy?
A thyroidectomy is a surgical procedure to remove all or part of the thyroid gland and used to treat diseases of the thyroid gland including:
- Thyroid cancer
- Hyperthyroidism (overactive thyroid gland)
- Large goiters or thyroid nodules causing symptomatic obstruction such as swallowing or breathing difficulties.
- Multi-nodular Goiter
A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
Thyroid Surgery: FAQ
Why do I need a Total Thyroidectomy vs. Lobectomy?
In general, at UCSF and most of the United States, when a diagnosis of cancer is known BEFORE the operation a total thyroidectomy is warranted. If there is not a clear diagnosis at the time of the operation half of the thyroid may be removed (lobectomy) for a final diagnosis. If cancer is found after the initial operation, reoperation depends on what the final pathology shows.
What if my biopsy results are “Atypical Follicular Lesion of Undetermined Significance”, "Follicular neoplasm", "Indeterminate", or "Non-diagnostic"?
In the case of these biopsy results, a thyroid lobectomy is indicated. Confirmation of a benign or malignant thyroid mass can only be done after removal of the affected thyroid lobe. Pathologists have to look at very thin slices of the tissue to make a diagnosis. If a diagnosis of cancer is confirmed (usually about 7-10 days following your operation), a second operation to remove the other lobe of the thyroid (completion thyroidectomy) may be needed.
What is Frozen Section and when is it used?
Frozen section is a biopsy done during the operation. It is useful if you have had a suspicious biopsy prior to the operation or if a lymph node is found during the operation that does not appear to be normal. The frozen section can then be used to determine a diagnosis of cancer. If cancer is diagnosed, then a total thyroidectomy and possible removal of surrounding lymph nodes would be indicated. Frozen section is NOT useful for follicular adenoma, indeterminate, or non-diagnostic biopsy results.
What are the risks of the operation?
There are three main risks for total thyroidectomy.
- Recurrent laryngeal nerve injury: This nerve controls your vocal cords and if injured you will have a hoarse voice. There is a 1% chance of permanent hoarseness and a 5% chance of temporary hoarseness (<6months).
- Low blood calcium: There are parathyroid glands that lie behind your thyroid gland that help to control your blood calcium levels. If they are injured or removed (can lie within the thyroid gland) during your operation, then your blood calcium can be too low. This would require you to take calcium and vitamin D supplementation. There is a 1% chance of permanent calcium supplementation and 5% chance of temporary calcium supplementation.
- Bleeding: There is a 1/300 risk of bleeding with your operation. This is the main reason you stay overnight in the hospital.
How do I prepare for surgery?
There is no reason to change your diet and/or most medications prior to your operation. You will be seen by the anesthesiologist at least one week prior to your surgery for a preoperative check. At this appointment there may be blood or other tests done to prepare you for your surgery. If you take blood thinning medications, such as aspirin, Plavix, ibuprofen, or Coumadin, you will need to contact the prescribing physician to discuss stopping these medications prior to your surgery.
Do I need to donate blood (autologous or designated donor) prior to my surgery?
It is highly unlikely that you will require a blood transfusion during your thyroidectomy, and therefore not medically necessary to donate (autologous or designated donor) blood prior to your surgery.
How long is my hospital stay? Can I have someone stay with me overnight?
Most patients only spend a maximum of one night in the hospital. There is no guarantee for a private room.
The incision is about 1-2 inches in length, and is placed in the midline of the neck in a normal skin crease to minimize scarring and visibility.
How do I care for the incision?
There will be Steristrips or surgical glue on your incision. These can be removed 10-14 days following your operation. There is no need to place any further dressing on your incision. You may use vitamin E oil or similar product to help the healing process, but it is NOT necessary. You SHOULD use sunscreen and/or cover to protect the incision from the sun. You may take a shower and get it slightly wet but not soaking wet.
What medications will I be taking after my operation?
If you have had a total thyroidectomy, you will need to take thyroid hormone (Levoxyl or Synthroid) for the rest of your life because you no longer have a thyroid gland to supply the necessary hormone. Thyroid hormone has a long half-life and it takes about 6-8 weeks from starting or changing your medication dose to determine if you need a change in dosage. In general, once you are on the correct dose you remain on the same dose for life. If you become pregnant, your dose will most likely need to be increased. Management of your thyroid hormone is done through blood test (TSH) by your Endocrinologist or Primary Care Physician. If your calcium level is low or you have symptoms of low blood calcium, you may have to take calcium supplementation following thyroidectomy.
Are there any restrictions following my operation?
You can resume regular activity as tolerated. Walking outside, going up and down stairs, and performing light activities are all encouraged. Avoid strenuous activity or lifting anything that weighs 10 pounds or more until you feel up to it. If you are feeling well and are not taking any pain medication, you may drive (usually the third or fourth day after surgery).
When can I expect to return to work?
In general, you can return to work when you feel ready, usually within one to two weeks.
Are there any dietary restrictions following my surgery?
Resume a normal balanced diet as tolerated. Be sure to drink plenty of fluids.
When should I have my post-operative appointment?
You should be seen by your surgeon approximately 2-4 weeks following your surgery. This appointment can be made by calling the surgeon's office when you return home following your surgery.
When can I expect my pathology results?
In general, pathology results can expect to be final approximately 7-10 days. This may vary depending on the type of surgery. Special staining may be necessary and may delay results. Pathology results will be discussed at your post-operative appointment unless otherwise indicated.
How do I know if I need any further treatment?
If applicable, further treatment questions will be addressed at your post-operative appointment with the surgeon. Treatment options may also be discussed with your referring Endocrinologist.
