About Diabetes
Diabetes, defined as elevated blood sugar, is a disorder of metabolism, i.e., the way the body uses digested food for growth and energy. If not controlled, diabetes can be life-threatening, and is associated with long-term complications that can affect every system and part of the body. Diabetes is classified into different types, based on various causes.
Types of Diabetes
Type 1 diabetes (previously called “juvenile diabetes”) is an autoimmune disorder, in which the insulin producing beta cells are destroyed by the body’s immune system. As a result the body cannot produce insulin, the hormone that allows glucose to enter and fuel the cells. To survive, individuals with type 1 diabetes must take insulin every day. It is estimated that 5 to 10% of Americans who are diagnosed with diabetes have type 1 diabetes.
Type 2 diabetes (previously called “adult onset diabetes”) is the most common type of diabetes, accounting for 90 to 95% of all diabetes. In type 2 diabetes, the body does not produce enough insulin and/or the body’s cells become resistant to insulin.
Gestational diabetes occurs in some women who have high blood glucose levels during pregnancy but have never had diabetes. It affects about 4% of all pregnant women, with about 135,000 cases in the United States each year. Women who have gestational diabetes have a 20 to 50% chance of developing type 2 diabetes in the next five to ten years.
Impact of Diabetes
Type 2 diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, peripheral artery disease (PAD), and nerve damage due to diabetic peripheral neuropathy.
About 80 percent of people with Type 2 diabetes are overweight. Of those, some are severely or morbidly obese. A standard way to define overweightness, obesity, and morbid obesity is with the body mass index (BMI), a measure of body fat based on height and weight. The average BMI is 25. Morbid obesity is defined as the following:
- A BMI of 40.0 or higher is considered severely (or morbidly) obese
- A BMI of 35.0 or higher in the presence of at least one other significant co-morbidity (diabetes, coronary artery disease, hypertension, sleep apnea, or degenerative joint disease) is also classified as morbid obesity.
An individual can determine whether they are obese or morbidly obese using a BMI calculator.
Glucose Metabolism and Diabetes
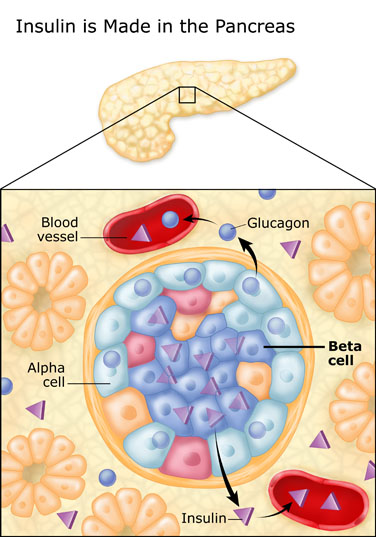
Most of the food people eat is broken down into glucose, the form of sugar in the blood. Glucose is the main source of fuel for the body. After digestion, glucose passes into the bloodstream, where it is used by cells for growth and energy. For glucose to get into cells, insulin must be present. Insulin is a hormone produced by the pancreas, a large gland behind the stomach.
|
|
| ImageCourtesy of UCSF Diabetes Education Online |
The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas produce juices that help digest food, and hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body to use and store energy from food.
Throughout the pancreas are clusters of cells called the islets of Langerhans. Islets are made up of several types of cells, including beta cells that make insulin. Insulin is a hormone that helps the body use glucose for energy.
Insulin and Type 2 Diabetes
Diabetes develops when the body doesn't make enough insulin, cannot use insulin properly, or both, which causes glucose to build up in the blood. Diabetes is a serious disease which can be life threatening if it is not controlled. It is often associated with long-term complications that can affect every system and part of the body. Diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, amputation, and nerve damage.
When a person eats, the pancreas automatically produces the right amount of insulin to move glucose from blood into the cells. In people with Type 2 diabetes, the cells do not respond appropriately to the insulin that is produced. Glucose builds up in the blood, overflows into the urine, and passes out of the body in the urine. Thus the body loses its main source of fuel even though the blood contains large amounts of glucose.
When type 2 diabetes is diagnosed, the pancreas is usually producing enough insulin, but for unknown reasons the body cannot use the insulin effectively, a condition called insulin resistance. After several years, insulin production decreases. The result is the same as for type 1 diabetes--glucose builds up in the blood and the body cannot make efficient use of its main source of fuel.
Who Develops Type 2 Diabetes
About 90 to 95 percent of people with diabetes have Type 2. The symptoms of type 2 diabetes develop gradually. Symptoms may include fatigue, frequent urination, increased thirst and hunger, weight loss, blurred vision, and slow healing of wounds or sores. Some people have no symptoms.
Type 2 diabetes is most often associated with older age, obesity, family history of diabetes, previous history of gestational diabetes, physical inactivity, and certain ethnicities. Type 2 diabetes is increasingly being diagnosed in children and adolescents, especially among African American, Mexican American, and Pacific Islander youth.
How is diabetes diagnosed?
The fasting blood glucose test is the preferred test for diagnosing diabetes in children and nonpregnant adults. The test is most reliable when done in the morning. However, a diagnosis of diabetes can be made based on any of the following test results, confirmed by retesting on a different day:
- A blood glucose level of 126 milli grams per deciliter (mg/dL) or higher after an 8-hour fast. This test is called the fasting blood glucose test.
- A blood glucose level of 200 mg/dL or higher 2 hours after drinking a beverage containing 75 grams of glucose dissolved in water. This test is called the oral glucose tolerance test (OGTT).
- A random--taken at any time of day--blood glucose level of 200 mg/dL or higher, along with the presence of diabetes symptoms.
How is diabetes managed?
Healthy eating, physical activity, and blood glucose testing are the basic management tools for type 2 diabetes. In addition, many people with type 2 diabetes require one or more diabetes medicines--pills, insulin, and other injectable medicine--to control their blood glucose levels.
Adults with diabetes are at high risk for cardiovascular disease (CVD). In fact, at least 65 percent of those with diabetes die from heart disease or stroke. Managing diabetes is more than keeping blood glucose levels under control--it is also important to manage blood pressure and cholesterol levels through healthy eating, physical activity, and the use of medications, if needed. By doing so, those with diabetes can lower their risk. Aspirin therapy, if recommended by a person's health care team, and smoking cessation can also help lower risk.
People with diabetes must take responsibility for their day-to-day care. Much of the daily care involves keeping blood glucose levels from going too low or too high. When blood glucose levels drop too low--a condition known as hypoglycemia--a person can become nervous, shaky, and confused. Judgment can be impaired, and if blood glucose falls too low, fainting can occur.