Perianal and Perirectal Abscess/Fistula
What causes perianal abscess?
Perianal abscess is a superficial infection that appears as a tender red lump under the skin near the anus. The infection occurs when bacteria gets trapped in the crypt glands that line the anal canal. The bacteria and fluid (pus) build up and becomes a lump that is red and painful (like a “pimple”). This type of abscess happens most often in male babies under a year of age. It may drain pus on its own and then heal and disappear.
What causes perirectal abscess?
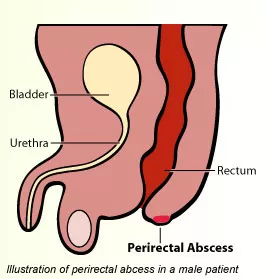
Perirectal abscess is different from perianal abscess. Perirectal abscess is an infection that is deep and tracks up along the rectum into the pelvis and are very rare in healthy newborns and children. These deep abscesses can be found in various locations in the pelvis (see figure) and can be associated with inflammatory bowel disease, such as Crohn’s disease.
What is a fistula?
Perianal and perirectal abscesses can be associated with fistula development. Fistula is a tube-like connection between the space inside the anus (anal canal or rectum) and the skin outside the anus. Once a fistula forms, bacteria from the intestine becomes trapped and causes the infection to return. Fistula that forms from perianal abscess is superficial. Fistula that forms from perirectal abscess is deep and can track through the different layers of the pelvic floor muscle and anal sphincter muscle complex.
How is perianal or perirectal abscess diagnosed?
Perianal abscess is diagnosed on physical examination. No other imaging study is necessary. Babies can be irritable and fussy. The abscess may be firm, red, and tender to the touch. If left untreated, the infection can spread locally to the buttock area.
Children with perirectal abscess can appear sicker with fever and pain. The location of the abscess can be not determined by physical examination and requires additional X-ray study, either CT scan or MRI of the pelvis.
How is perianal abscess/fistula treated?
Perianal abscess can sometimes be treated at home with Sitz baths or warm water soaks with each bowel movement or at least 2-3 times a day. The abscess can drain pus on its own and then heal without needing any other treatment. When the infection has spread locally to the surrounding buttock area, antibiotics are prescribed to treat the skin infection. In addition, an abscess that does not drain by itself may need to be drained in the office by the pediatric surgeon. This may be all that is needed to treat the abscess and allow the skin to heal permanently. Perianal abscess may return and require repeated warm water soaks or drainage. However, in most healthy babies, the problem will go away completely at one year of age.
For those babies who have repeat infections, there may be a fistula that has formed and is causing bacteria contamination and abscess development. Your child’s pediatric surgeon will discuss the option of fistulotomy. This an operation that is done in the operating room with your child under general anesthesia. The operation is an outpatient procedure and your child will go home the same day. During the operation, the pediatric surgeon identifies the opening in the anal canal that connects to the opening in the skin. The tube-like connection is cut opened. The incision that is made during the fistulotomy is left open and not closed with stitches. This open wound will heal and close by itself in one to two weeks. While the area is healing, no infection will occur in the wound, even though your child has bowel movements. You can help keep the area clean by giving your child a warm bath after every bowel movement. This will clean and soothe the area while it is healing. Antibiotic is not needed at this time. Prescription pain medication is not routinely required after this operation. Children usually only need acetaminophen (Tylenol®) or ibuprofen (Motrin®) once they are at home.
How is perirectal abscess/fistula treated?
Location and size of the perirectal abscess determines what needs to be done to the treat the infection. When the abscess is small, antibiotics alone are enough to treat the infection. However, when the abscess is large, in addition to antibiotics, the infection will need to be drained. Drainage procedure can be done by radiologist who will place a drain (small plastic tube) into the abscess to drain the pus. The infection can also be drained by the pediatric surgeon in the operating room. The type of procedure that is done will depend on the location of the abscess. Both types of procedure are done with your child under general anesthesia. After the procedure, your child will be admitted to the hospital for a few days until the infection has resolved. Sometimes, patients are discharged home with drain in the place, which can be removed in the clinic.
Perirectal abscess can be associated with fistula. The fistula can be identified on the CT or MRI scan that was used to diagnose the perirectal abscess. If perirectal abscess or fistula is identified, your child will need to be seen by pediatric gastroenterologist to be evaluated for inflammatory bowel disease. If your child is diagnosed with inflammatory bowel disease, medications will be prescribed to treat the inflammation and allow the fistula to heal. In some occasions, the fistula stays open and continues to cause abscess formation. To prevent future abscess, your child’s pediatric surgeon may recommend an operation to place a Seton (thin rubber band) through the fistula to prevent bacteria and pus from building up. After this operation, your child can go home the same day or may need to be admitted in the hospital for a few days depending on the extent and how deep the fistula is located. The Seton can remain in place for few months. The decision to remove the Seton is determined by your child’s pediatric gastroenterologist and pediatric surgeon. When the Seton needs to be removed, removal can be done in clinic.
