Carotid Stenting
Vascular surgeons at UCSF have over five decades of proven experience in preventing strokes with carotid artery surgery, and in treating rare disorders of the carotid arteries such as fibromuscular dysplasia. The UCSF Vascular Surgery Program has also earned the highest designation for quality outcomes in carotid artery surgery by the Leapfrog Initiative that compared outcomes in carotid artery surgeries throughout Northern California.
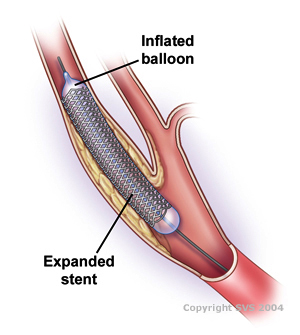
Carotid artery stenting is a procedure in which a vascular surgeon inserts a slender, metal-mesh tube, called a stent, which expands inside your carotid artery to increase blood flow in areas blocked by plaque.
Your carotid arteries are located on each side of your neck and extend from your aorta in your chest to the base of your skull. These arteries supply blood to your brain. You have one main carotid artery on each side, and each of these divides into two major branches, the external and the internal carotid arteries. The external carotid supplies blood to your face and scalp. Your internal carotid artery is more important because it supplies blood to the brain.
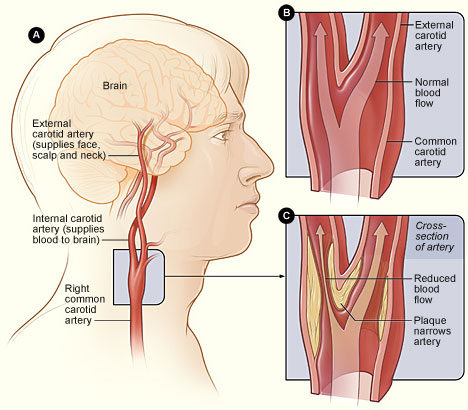
Figure A shows the location of the right carotid artery in the head and neck. Figure B shows the inside of a normal carotid artery that has normal blood flow. Figure C shows the inside of a carotid artery that has plaque buildup and reduced blood flow.
Hardening of the arteries (called atherosclerosis) can cause a build-up of plaque, which builds up in the walls of your arteries as you age. Cholesterol, calcium, and fibrous tissue make up the plaque. As more plaque accumulates, your arteries can narrow and stiffen. Over time enough may build up to reduce blood flow through your arteries, or cause blood clots or pieces of plaque to break free and to block the arteries in the brain beyond the build-up.
During the carotid stenting procedure, your physician inserts a stent into your carotid artery after performing angioplasty. Angioplasty uses a balloon inflated in the narrowed part of the artery to open it. Using a catheter, the surgeon guides a compressed stent to the affected area in your carotid artery. Once the stent is in place, the surgeon releases it. The stent then expands to fit the artery. In most cases, your physician then uses a balloon catheter to further expand the stent. Stents remain permanently in your carotid artery. Carotid stenting usually takes about 1-2 hours, but may take longer in some circumstances.
Risk Factors for Complications
Blockage by a clot or other debris in an artery in your brain, called an embolism, is the most serious complication that can occur after carotid stenting. This blockage can cause a stroke. Other complications that may cause a stroke include a blood clot forming along the stent or a tear in the artery wall called a dissection. The re-blockage of the carotid artery, called restenosis, is another possible complication. The dye used for the angiogram can sometimes cause damage to the kidneys, especially in people who already have kidney trouble. Bleeding from the puncture site in the groin or arm artery, called a hematoma or a false aneurysm, can also occur, but this is unusual. Bruising and mild tenderness at the puncture site is common, however, and usually resolves with time.
You may not be a candidate for carotid stenting if you have one or more of the following:
- A life expectancy shorter than 2 years
- Complete obstruction of the carotid artery
- Irregular heart beat
- Allergy to procedural medications
- Bleeding in your brain within the last 2 months
Factors that may increase your chance for having complications during carotid stenting may include:
- High blood pressure
- An allergy to contrast dye
- Sharp bends or other anatomies in the carotid arteries
- Significant plaque or atherosclerosis of the aorta near the beginning of the carotid artery
- An age more than 80 years
- Extensive blockages in the arm and leg arteries
- Poor kidney function
What can I do to stay healthy?
Although carotid stenting opens your artery and keeps blood flowing, it does not stop plaque from building up. To prevent hardening of the arteries from occurring again, you should consider the following changes:
- Eat more foods low in saturated fat, cholesterol, and calories
- Exercise regularly, especially aerobic exercises such as walking
- Maintain your ideal body weight
- Quit smoking
- Follow your physician's recommendations for medications to control cholesterol and to thin the blood
