Pancreas Transplant
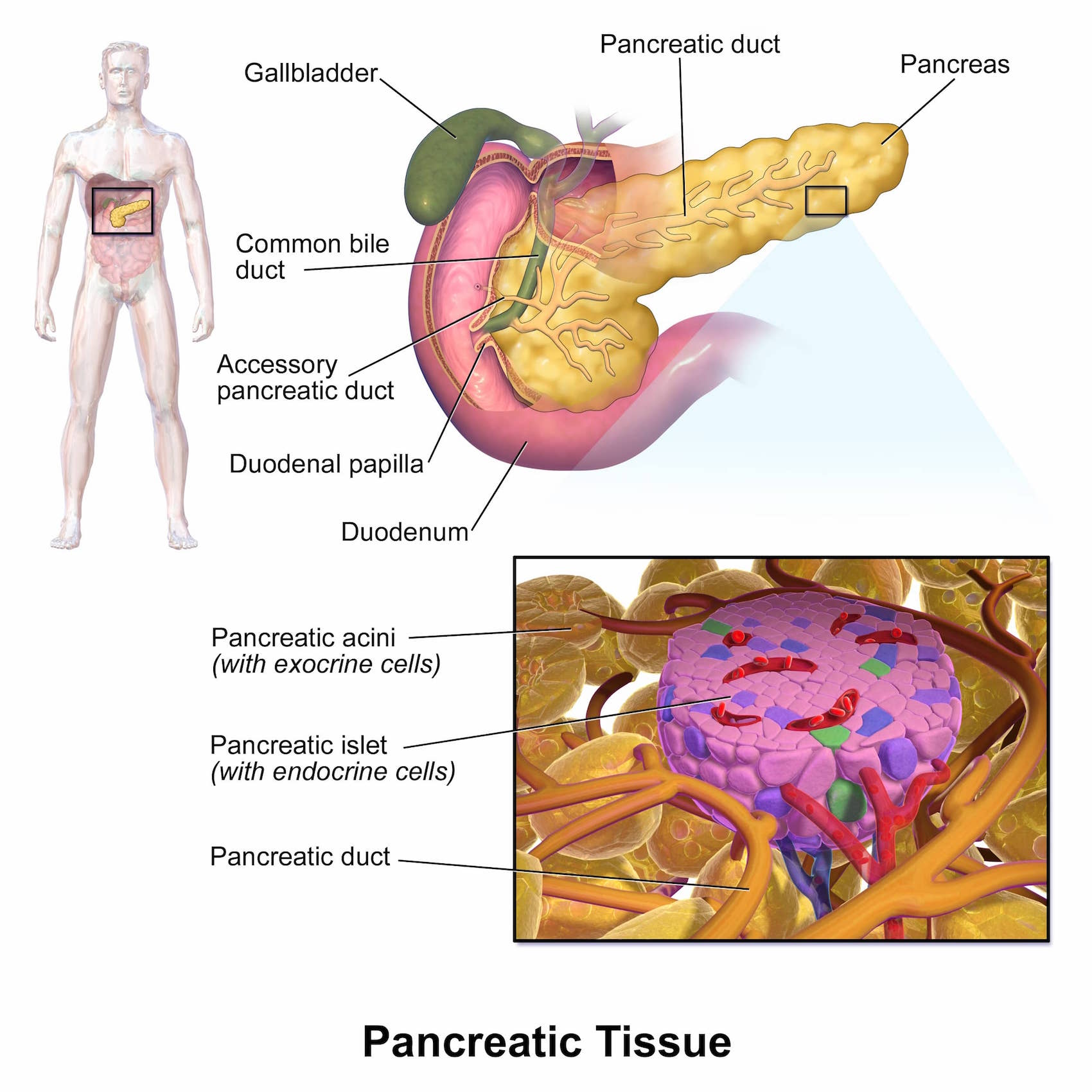
The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas produces juices that help digest food and hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body to use and store energy from food.
A pancreas transplant is an organ transplant that involves implanting a healthy pancreas (one that produces insulin) into a person whose pancreas no longer can supply sufficient insulin to the body. The healthy pancreas comes from either a deceased donor, or in the form of a partial pancreas from a living donor.
A pancreas transplant offers a potential cure for type 1 or insulin-dependent diabetes. A successful pancreas transplant will eliminate the need for insulin injections, reduce or eliminate dietary and activity restrictions due to diabetes, and decrease or eliminate the risk of severe low blood sugar reactions. A pancreas transplant can also help manage the damage to other organs including the kidneys that may result from type 1 diabetes.
Pancreas transplants are primarily offered to persons with type 1 with severe kidney disease or other life-threatening consequences from uncontrolled glucose levels. Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Beta cells (β cells) are a type of cell found in the pancreatic islets of the pancreas. They make up 65-80% of the cells in the islets.
Who Gets Pancreas Transplants
Patients with type 2 diabetes are generally not offered pancreas transplants because their disease results from the body's inability to use insulin properly, not from an inability to produce in insulin in the pancreas. While the beta cells in type 2 patients may become exhausted and fail, the same fate might await beta cells in transplanted pancreas due to the same factors that caused insulin resistance in the first place.
Type 1 Diabetes
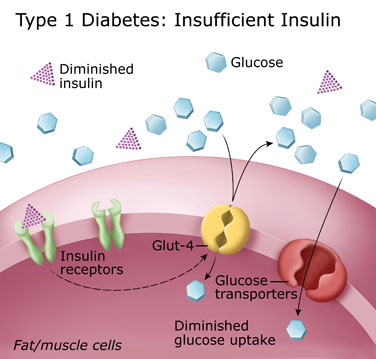 As noted above, Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Damage to beta cells results in an absence or insufficient production of insulin produced by the body. Most cases of type 1 diabetes have an autoimmune basis where the immune system mistakenly attacks and destroys beta cells.
As noted above, Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Damage to beta cells results in an absence or insufficient production of insulin produced by the body. Most cases of type 1 diabetes have an autoimmune basis where the immune system mistakenly attacks and destroys beta cells.
People with type 1 diabetes have very little or no insulin and need to take insulin everyday. Insulin therapy is life-saving. However, most people with type 1 diabetes continue to have blood glucose levelsabove normal. This puts them at risk for the long-term complications of diabetes such as diabetic retinopathy, an eye disease that can cause poor vision and blindness, and diabetic nephropathy, a kidney disease that can lead to kidney failure.
Some people have what doctors call labile, or brittle, diabetes. Blood glucose levels swing from high to low despite the best insulin plans. Those who are able to keep their blood glucose levels near normal often have trouble with low blood glucose (hypoglycemia).
Over time, some type 1 diabetics lose awareness of the early symptoms that warn them that their blood glucose level is dropping. This is called hypoglycemia unawareness and raises the risk of severe hypoglycemia. Hypoglycemia unawareness is a life-threatening condition that is not easily treatable with medication and is characterized by reduced or absent warning signals for hypoglycemia. Some Type 1 diabetic patients have been known to set their alarms to wake them several times a night out of fear they may have a catastrophic hypoglycemic episode while asleep.
Considerations in Patients Considering Pancreas Transplants
Although a pancreas transplant offers a potential cure for type 1 diabetes, the side effects of anti-rejection medications required after transplant can be more serious than type 1 diabetes itself. Therefore the risks of the transplant must be outweighed by benefits of getting the transplant. When one of more the following apply, a pancreas transplant may be considered a viable treatment option.
- Type 1 diabetes not controlled with standard treatment
- Frequent severe insulin reactions
- Very poor blood sugar control
- Hypoglocemia Unawareness (see above)
- Severe kidney damage
Types of Pancreas Transplants
There are three main types of pancreas transplantation:
- Pancreas transplant alone, for the patient with type 1 diabetes who usually has severe, frequent hypoglycemia, but adequate kidney function.
- Simultaneous pancreas-kidney transplant (SPK), when the pancreas and kidney are transplanted simultaneously from the same deceased donor. One of the most serious complications of type 1 diabetes is end-stage renal disease (ESRD) or end-stage kidney disease, which may require a kidney transplant. A kidney transplant without a pancreas transplant means you must take antirejection medication for the kidney and continue to take insulin.The possibility of diabetes damaging the new kidney and other organs also remains. Successful combined kidney-pancreas transplants prevent diabetic damage in newly transplanted kidneys as well as eliminate the need for insulin therapy. In the best case scenario, a patient would receive a new kidney and pancreas from the same donor.
- Pancreas-after-kidney transplant (PAK), when a cadaveric, or deceased, donor pancreas transplant is performed after a previous, and different, living or deceased donor kidney transplant.
