Diabetic Foot Ulcers
The UCSF Center for Limb Preservation & Wound Care is the first in the Bay Area to focus on amputation prevention and high-risk diabetic patients. We save limbs because we offer efficient, coordinated care with a high level of expertise, and because we are aggressive in our goal of preserving a functional foot.
A diabetic foot ulcer is an open sore or wound on the foot of a person with diabetes, most commonly located on the plantar surface, or bottom of the foot. Diabetic foot ulcers occur in approximately 15% of persons with diabetes. Of those who develop a foot ulcer, 6% will be hospitalized due to infection or other ulcer-related complication. The risk of foot ulceration and limb amputation increases with age and the duration of diabetes.
Diabetes is the leading cause of non-traumatic lower extremity amputations in the U.S. Between 14-24% percent of patients with diabetes who develop a foot ulcer will require an amputation, and foot ulceration precedes 85% of diabetes-related amputations. In the U.S., 82,000 amputations are performed each year on persons with diabetes, half of those age 65 or older.
The good news is that a foot ulcer is preventable if the underlying conditions causing it, diabetic peripheral neuropathy and/or peripheral arterial disease, are appropriately diagnosed and treated.
Causes
Peripheral neuropathy (nerve damage) and lower extremity ischemia (lack of blood flow) due to peripheral artery disease are the primary causes of diabetic foot ulcers.
Diabetic Peripheral Neuropathy
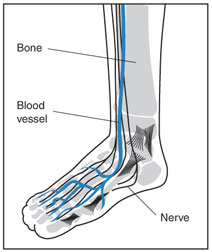 Diabetic peripheral neuropathy is a precipitating factor in almost 90% of diabetic foot ulcers. Chronically high glucose (blood sugar) levels damage nerves, including the sensory, motor and autonomic nerves. Diabetic neuropathy also damages the immune system and impairs the body's ability to fight infection.
Diabetic peripheral neuropathy is a precipitating factor in almost 90% of diabetic foot ulcers. Chronically high glucose (blood sugar) levels damage nerves, including the sensory, motor and autonomic nerves. Diabetic neuropathy also damages the immune system and impairs the body's ability to fight infection.
Sensory nerves enable people to feel pain, temperature, and other sensations. When sensory nerves of a diabetic person are damaged (sensory neuropathy), they may no longer be able to feel heat, cold, or pain in their feet. A cut or foot sore, a burn from hot water, or exposure to extreme cold might go completely unnoticed because of numbness and lack of sensation. The sore or exposed area may then become infected and not heal properly due to the body's impaired ability to fight infection.
Peripheral neuropathy also causes muscle weakness and loss of reflexes, especially at the ankle. This may change the way a person walks and lead to foot abnormalities and deformities such as bunions, hammertoes, and charcot foot. These play an important role in the pathway of diabetic foot ulcers since they contribute to abnormal pressures in the plantar area (heel and bottom) of the foot, predisposing it to ulceration.
Shoes that no longer fit due to abnormalities and deformed foot structure may rub against toes causing blisters and ulcers on areas of the foot that are numb due to sensory neuropathy. If not treated promptly, an ulcer may become infected and spread to the bone causing osteomyelitis, a serious complication that might require surgery.
 |
 |
 |
Autonomic dysfunction causes decreased sweating resulting in cracked skin and ulceration, making the skin vulnerable to infection.
Peripheral Artery Disease
Diabetes also damages blood vessels by causing inflammation and atherosclerosis, or hardening of the arteries. Narrowing of the arteries causes ischemia, a condition in which the blood circulation in the arteries is restricted and the availability of oxygen, glucose, and critical nutrients to tissues in the body is substantially reduced. When poor circulation affects the arteries of the feet and hands, it is called peripheral artery disease, or PAD. By restricting the supply of oxygenated, nutrient-rich blood to the site of the ulcer, peripheral artery disease increases the risk an ulcer will become infected and heal slowly--or not at all.
Peripheral artery disease (PAD) is 2–8 times more common in patients with diabetes, and about half of patients with a diabetic foot ulcer will also be found to have co-existing PAD. Identifying PAD in patients with foot ulceration is important because its presence is associated with slower (or lack of) healing of foot ulcers as well as other serious complications. Diagnosing PAD is challenging in patients with diabetes, as they frequently lack typical symptoms, such as intermittent claudication (rest pain), even in the presence of severe tissue loss.
Diabetes patients tend to develop vascular disease particularly in the peripheral arteries of the feet and legs. Michael S. Conte, M.D., Chief of Vascular Surgery at UCSF, discusses the connection between peripheral artery disease (PAD) and diabetes.
Types of Diabetic Ulcers
There are several types of diabetic foot ulcers
- Neuropathic ulcers occur where there is peripheral diabetic neuropathy, but no ischemia caused by peripheral artery disease.
- Ischemic ulcers occur where there is peripheral artery disease present without the involvement of diabetic peripheral neuropathy.
- Neuroischemic ulcers occur where the person has both peripheral neuropathy and ischemia resulting from peripheral artery disease.
Arriving at the correct diagnosis and identifying the cause of a diabetic ulcer is critical since it affects the treatment plan.
Risk Factors
As noted earlier, diabetic peripheral neuropathy and peripheral artery disease (PAD) are strong risk factors associated with the development of diabetic foot ulcers. Other risk factors include cigarette smoking, poor glycemic (sugar) control, and previous foot ulcerations. In addition, certain groups have a greater risk of developing foot ulcers including Native Americans, African Americans, Hispanics, older men, insulin-dependent diabetics, and persons with diabetes-related kidney, eye, and heart disease.
Signs and Symptoms
Common signs and symptoms of a diabetic foot ulcer include:
- Appearance of drainage on the person's socks
- Redness and swelling in the area
- Odor if the ulcer has progressed significantly
Treatment
A diabetic foot ulcer acts as a portal for systemic infections such as cellulitis, infected foot ulcers, and osteomyelitis. These are especially dangerous to patients with diabetes, whose impaired immunity increases their risk for local and systemic infection. Therefore, debridement and antibiotic therapy should be initiated as soon as possible. Blood sugar should also be monitored closely and controlled, because hyperglycemia may increase the virulence of infectious microorganisms.
The goal of treatment is to accelerate the healing process and decrease the chance for infection (or prevent a recurrence of infection). Treatment usually consists of:
- Optimal glucose control.
- Debridement - removal of all hyperkeratotic (thickened) skin, infected and nonviable, including necrotic (dead), tissue, slough, foreign debris, and residual material from dressings.
- Systemic antibiotics for deep infection, drainage, and cellulitis.
- Off-loading - Relieving the pressure from the ulcerated areas by having the patient wear special foot gear, a brace, specialized castings, or using a wheelchair or crutches.
- Creating a moist wound environment.
- Treatment with growth factors and/or cellular therapy if the wound is not healing.
Wound Care
- Wounds and ulcers heal faster and have a lower risk of infection if they are kept covered and moist, using dressings and topically-applied medications.
- Products including saline, growth factors, ulcer dressings, and skin substitutes are highly effective in healing foot ulcers.
- There should be adequate circulation to the ulcerated area.
- Tight control of blood glucose is critical during to the effect treatment of a diabetic foot ulcer. This will enhance healing and reduce the risk of complications.
Surgical Options
Many non-infected foot ulcers are treatable without surgery. However, surgery may be required to:
- Remove pressure on the affected area, including shaving or excision of bone(s).
- Correct deformities, such as hammertoes, bunions, or bony “bumps.”
- Treat infections such as osteomyelitis, an infection of the bone, by surgically removing the infected bone.
Healing time may range from weeks to several months, depending on:
- Wound size and location
- Pressure on the wound from walking or standing
- Degree of swelling
- Issues with proper circulation
- Blood glucose levels
- What treatments are being applied to the wound
Risk Reduction
The risk of developing a foot ulcer can be reduced by:
- Smoking cessation
- Lowering consumption of alcohol
- Reducing high cholesterol
- Controlling blood glucose levels
- Wearing the appropriate shoes and socks
- Inspecting feet every day—especially the sole and between the toes—for cuts, bruises, cracks, blisters, redness, ulcers, and other signs of abnormality
