Charcot Foot
Charcot foot is a progressive condition that involves the gradual weakening of bones, joints, and soft tissues of the foot or ankle. Charcot foot is a severe complication of diabetes and is caused by peripheral neuropathy (nerve damage) in which the person's foot or ankle becomes insensate (insensitive to pain). The condition is thought to be caused by repetitive injury, typically a series of microtraumas a person may only be minimally or even completely unaware of.
As Charcot foot progresses, the bones can become so weakened that they fracture. Joints may dislocate in the foot or ankle. With repetitive trauma and degeneration, the joints in the foot may eventually collapse, causing the foot to become deformed and take on an abnormal shape such as a rocker-bottom appearance. The deformity can lead to foot sores and ulcers, bone infection (osteomyelitis), and if not treated aggressively, amputation.
While Charcot's foot has been thought to be a rare condition, its true prevalence may be underestimated because of a mistaken or delayed diagnosis. Further, the incidence of Charcot foot may be increasing in step with the epidemic of new diabetes cases in the U.S. and worldwide. Because of its potentially devastating impact, people with diabetes need to take preventive measures and seek immediate care if symptoms appear, preferably at a multidisciplinary program with excellence in vascular surgery and podiatric care. Early diagnosis and management are critical to avoiding the rapid progression towards permanent foot deformation and its associated complications.
Other Names
- Charcot foot and ankle
- Charcot Arthropathy (Arthropathy is a disease of the joints)
- Charcot Neuro-Arthropathy (CN)
Causes and Clinical Course
Charcot foot can develop when a person sprains or breaks a bone in their foot or ankle and the injury goes untreated due to a lack of sensation caused by peripheral neuropathy. The person continues to walk on the broken foot, causing trauma to the bone. As part of the body's natural reaction to trauma, the bone begins to lose calcium and other materials that keep bones strong.
Eventually, the bone loss causes changes in the structure of the foot and areas of the foot collapse. When the collapse occurs to the midfoot, it rounds the bottom of the foot into a so called rocker-bottom foot deformity. Depending on the location of the bone break, the toes can start to curve under like claws or the ankle can become deformed and unstable. Sharp edges of bone may put pressure on the skin, creating the risk of chronic skin sores. The end result — a combination of bone disintegration and trauma – is Charcot foot.
Charcot arthropathy (joint disease) may affect any part of the foot and ankle, including the midfoot, hindfoot, ankle, heel and forefoot. Multiple regions may be involved. Fractures and dislocations frequently involve several bones and joints, with extensive fragmentation and deformity.
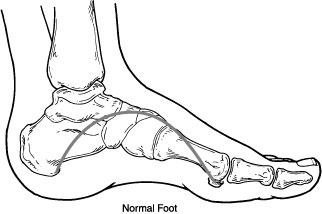
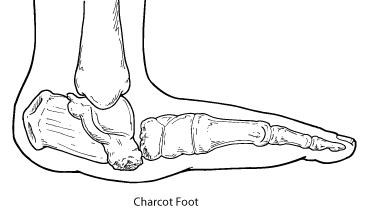
In Charcot foot, the joints in the foot collapse and the foot eventually becomes deformed.
Symptoms
The symptoms of Charcot foot may include:
- A foot that is warm to the touch and noticeably warmer than the opposite foot
- Redness
- Swelling
- Pain or soreness
Some Charcot joints, such as the ankle, may heal with fibrous tissue and this may result in gross instability (“floppy foot”) that may predispose the person to foot ulcers and may be difficult to support with braces.
Diagnosis
Early diagnosis of Charcot foot is important to stop foot structure deterioration. A detailed history will be taken and the foot and ankle will be examined for the classic signs of Charcot foot. X-rays and other imaging studies, as well as laboratory tests, may also be ordered.
Non-Surgical Treatment
Non-surgical treatment for Charcot foot consists of:
- Immobilization. Because the foot and ankle are so fragile during the early stage of Charcot, they must be protected so the weakened bones can repair themselves. Complete non-weightbearing is necessary to keep the foot from further collapsing. The patient will not be able to walk on the affected foot until the surgeon determines it is safe to do so. During this period, the patient may be fitted with a cast, removable boot, or brace, and may be required to use crutches or a wheelchair. It may take the bones several months to heal, although it can take considerably longer in some patients.
- Custom shoes and bracing. Shoes with special inserts may be needed after the bones have healed to enable the patient to return to daily activities, as well as helping prevent recurrence of Charcot foot, development of ulcers, and possible amputation. In cases with significant deformity, bracing is also required.
- Activity modification. A modification in activity level may be needed to avoid repetitive trauma to both feet. A patient with Charcot in one foot is more likely to develop it in the other foot, so measures must be taken to protect both feet.
Surgery
In some cases, the Charcot deformity may become severe enough that surgery is necessary. Surgical options may include realignment osteotomy and fusion (correction of deformity), or ostectomy (removal of bony prominence that could cause an ulcer).
Preventive Care
The patient can play a vital role in preventing Charcot foot and its complications by following these measures:
- Keeping blood sugar levels under control can help reduce the progression of nerve damage in the feet.
- Get regular check-ups from a foot and ankle surgeon.
- Check both feet every day—and see a surgeon immediately if you notice signs of Charcot foot.
- Be careful to avoid injury, such as bumping the foot or overdoing an exercise program.
- Follow the surgeon’s instructions for long-term treatment to prevent recurrences, ulcers, and amputation.
