Renal Artery Disease
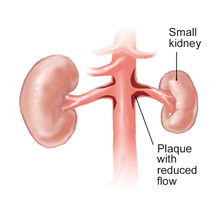
The renal arteries, like others in the human body, can become obstructed. Renal artery disease is usually caused by atherosclerosis, or hardening of the arteries due to the buildup of fatty deposits or plaques along the artery wall. This build-up can reduce blood-flow to one or both kidneys, or block flow completely depending on the location of the plaque. Decreased blood flow to the kidneys because of these blockages often causes hypertension (high blood pressure), and can lead to congestive heart failure and kidney failure.
Kidney Failure and Vascular Disease
 The kidneys cleanse the blood of waste products, balance the electrolytes in the body, control blood pressure and stimulate the production of red blood cells. They receive their blood supply through the renal arteries directly from the aorta, the largest artery that carries oxygen-rich blood from the heart to other organs in the body.
The kidneys cleanse the blood of waste products, balance the electrolytes in the body, control blood pressure and stimulate the production of red blood cells. They receive their blood supply through the renal arteries directly from the aorta, the largest artery that carries oxygen-rich blood from the heart to other organs in the body.
The kidneys are extremely sensitive to any decrease in blood flow. When a renal artery narrows due to plaque buildup (stenosis) and blood flow is restricted to even one kidney, high blood pressure (hypertension) can occur. Renal artery stenosis causes about 5% of all cases of hypertension and can reduce kidney size. When the stenosis involves both kidneys, it can also lead to impaired kidney function (renal failure). Stenosis of both renal arteries is a major cause of renal failure in the elderly.
Signs and Symptoms
High blood pressure that is not controlled by medications and lifestyle changes, including diet and exercise, may be a symptom of renal artery disease. Symptoms of renal artery disease may also include episodes of fluid retention or congestive heart failure. In some cases, renal artery disease may be entirely asymptomatic (not associated with any symptoms).
In severe cases, renal artery disease may lead to kidney failure. Symptoms of kidney failure include weakness, shortness of breath and fatigue.
Risk Factors
Many of the risk factors for renal artery disease are the same as those for atherosclerosis in other parts of the body, such as coronary artery disease and peripheral arterial disease. Risk factors for renal artery disease include:
- Age over 50
- Diabetes
- High cholesterol
- Smoking
- High blood pressure
- Family history of coronary artery disease, peripheral arterial disease, and/or renal artery disease
- Neurofibromatosis, a genetic disorder that disturbs cell growth in your nervous system, causing tumors to form on nerve tissue
Renal artery disease can also be caused by fibromuscular dysplasia (FMD). FMD results in the overgrowth of tissue inside the artery in a characteristic “chain of beads” pattern. This condition can affect other arteries, as well.
Diagnosis
Once a diagnosis of renal artery disease is suspected, a diagnostic test is generally ordered to evaluate the renal arteries for the presence of significantly narrowed areas. Tests that can be used to diagnose renal artery stenosis include abdominal duplex ultrasound, magnetic resonance angiography (MRA), and computed tomography (CTA).
Treatment and Surgery
The right treatment for an individual depends on the severity of the disease and the person’s medical history.
Lifestyle changes such as weight reduction, smoking cessation, exercise and a low-salt and low-fat diet can help slow or prevent renal artery disease. Medication to lower blood pressure is an important part of treatment, along with careful monitoring of the response to the blood pressure medications to be sure the blood pressure is lowered to the treatment goal.
For some patients with significant narrowing of the renal arteries, particularly patients with narrowed areas in the renal arteries on both sides of the body, or those with severe symptoms, a procedure may be recommended to open up the blocked arteries to restore circulation. In some cases, opening the blocked arteries may improve kidney function and may improve control of high blood pressure. Not surprisingly, the techniques used to open blocked renal arteries are very similar to those used to treat blocked coronary arteries.
Renal angioplasty
A small catheter – a long, thin tube – carrying a tiny balloon is inserted through a small puncture in the groin and guided by X-ray to the kidney artery. When the catheter is guided to the narrowed part of the artery, the balloon is inflated. As it expands, it compresses the plaque against the artery walls, re-opening the vessel for blood to flow through. Once the artery is open, the physician may insert a stent at the site to keep the artery open and support the arterial wall. Renal angioplasty can be done as an outpatient procedure or with only an overnight stay. It does not require general anesthesia, and has a short recovery period.
In certain cases, surgical treatment may be necessary to restore blood flow to the kidney and preserve kidney function. Surgical treatments for renal artery disease include:
- Endarterectomy, during which a vascular surgeon removes the diseased inner lining of the artery and the plaque deposits.
- Bypass procedure, which involves using a segment from another artery or vein to construct a detour around the blocked area of the renal artery. The most commonly used technique creates a bypass from the abdominal aorta (the large artery in the abdomen) to the kidney using a segment from the saphenous vein in the leg, or the hypogastric artery from the abdomen.
